No fear of anything: epilepsy, psychiatric comorbidity and surgery. A clinical case report
Introduction. Psychiatric conditions are common in patients with drug-resistant temporal lobe epilepsy. It can be extremely disabling, as it hinders the patient’s integration into society. Emotional symptoms may occur during crises or can be chronic and not directly related to seizures. Some of the most common disorders are depression, followed by anxiety disorders and obsessive symptoms such as phobias.
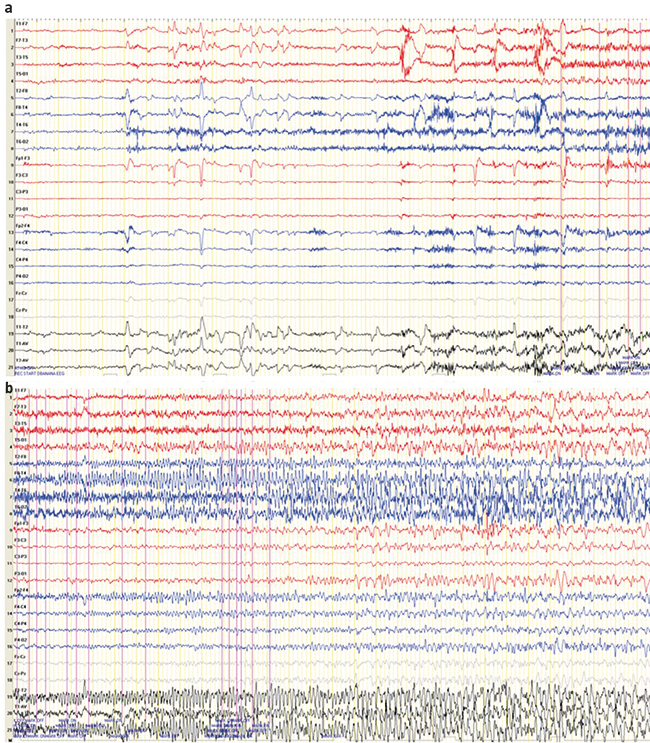
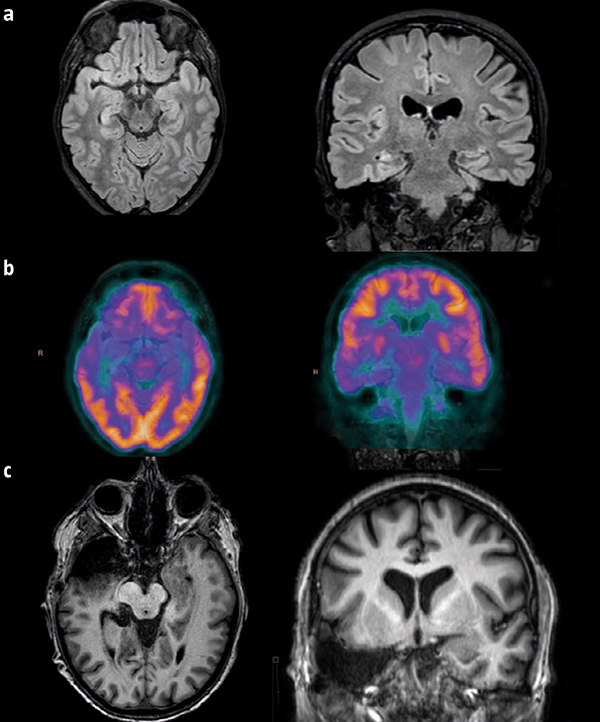
Case report. In the clinical case reported here, the patient suffers from drug-resistant focal epilepsy and psychiatric comorbidity (anxiety-depressive syndrome and phobias). In the pre-surgical evaluation, the origin of the seizures was established as the right mesial temporal region, and so surgery was performed. In check-ups, an improvement of both conditions was observed after surgery to treat her epilepsy.
Conclusion. The activation of the amygdala and its interaction with different brain structures seem to play an important role in emotional learning and aversive stimuli, thereby conditioning (depending on its pattern of activation) the individual’s ability to control their fear. There seems to be excessive activation in individuals with phobias. Surgical resection by anteromedial temporal lobectomy in patients with temporal lobe epilepsy is an effective treatment to achieve control over refractory seizures, and may also help to ease emotional symptoms, thus adding an extra benefit. A pre-surgical evaluation with a multidisciplinary approach can be used to predict post-operative neuropsychological change.
Key words. Alzheimer’s disease. Anticoagulation. Atrial fibrillation. Cognitive impairment. Dementia. Stroke.
|